Speech Breathing is Key for Speech Therapy Prevention in Kindergarten
Breathing is highly individual and the development of speech breathing largely determines how the child will speak. Proper control of breathing benefits the correctness of pronunciation, the ability to maintain fluency, normal lung volume and expressiveness of intonation in speech. In this article we discuss benefits of well-developed speech breathing and its correlation to speech delays. We also talk about 40 foundational learning toys and alternative activities that parents and child experts can use to boost lung capacity.
If parents adopt this holistic approach to breathing activities in the early childhood and preschool years on a systematic basis, it minimises needs for speech therapy in the future.
“Breath has patterns. Schemes create behaviour. Breath is a behaviour. Behaviour represents the person. Breath reveals the person.” (A. Muacevic & J. Adler, 2018)
1. What is speech breathing?
Breathing is the basis for life and human health. Normally, children in parallel with the physiological breathing form speech breathing. What is the difference? Physiological breathing, also called tidal breathing, is involuntary. Inhalation and exhalation have almost the same duration – 40% inhalation and 60% of passive exhalation, without activating muscles. Both are carried out through the nose. Whereas speech breathing encompasses a controlled process in which inhalation occurs through both the mouth and the nose, and the exhalation happens through the mouth with sounds, where inhale (10%) is shorter that exhale (90%) (Fuchs, S. & Rochet-Capellan, A., 2021). Hence, for speech – normal tidal breathing is not enough.
1.1. What is correct speech breathing?
Correct speech breathing ensures:
- normal vocalisation;
- a clear sound formation;
- maintenance of normal air volume, fluency, expressive intonation and pausing.
Pre-schoolers, especially children with disabilities often have unformed speech breathing, due to their age, height characteristics, somatic weakening and cranio-facial-nasal-oral differences (Hitos, S.F. et al., 2013). As a matter of fact, no correlation has been linked to specific gender differences (Hoit, J.D et al, 1990; Boliek C.A. et al, 2009).
This manifests itself in the following:
- weak inhale;
- insufficient volume of exhaled air; weak and short force of exhalation (speech sounds loud, then quiet, hardly audible);
- inadequate distribution of exhaled air. The child exhales the entire air supply on the first syllable and then finishes a phrase or word with a whisper. Or the child does not finish a word, “swallows” the end of a word or phrase).
- incorrectly directed exhaled air stream leads to distortion of sounds.
1.2. What type of breathing is important for speech breathing?
There are three main ways of breathing:
- upper respiration (clavicular breathing)
- middle respiration (thoracic or intercostal breathing)
- lower respiration (abdominal or diaphragmatic breathing)
For optimal voice usage and projection, proper breathing must come from the midsection or diaphragm. In other words, it is the lower breathing that provides most of the air volume for voicing.
Therefore, it is detrimental to form correct speech breathing of a child in a timely manner. Indeed, articulation flaws can be corrected in adulthood. However, can you imagine a healthy grown-up with speech impediments? Correction is a time-consuming process and the first impression still matters. It affects work life, social life and causes even behavioural and psychological issues.
Parents naturally want to set their children up for future success. Thus, we encourage mastering the “art of breathing” in order to bring an array of benefits for holistic healthy development.
2. Benefits of correct speech breathing for children
It is like riding a bicycle. Once a person learns how to “correctly” breathe, the person cannot unlearn it. Neuropsychological and neurophysiological correction is based on automatisation and rhythmitisation of the child’s body using basic multi-level breathing techniques. It generates a permanent effect and a qualitative change that will remain with the toddler and be ideally further developed before the age of 10 years, thereby reinforcing resilient control of breathing into adulthood.
- Breathing exercises improve the work of all the major systems of the body: cardiovascular, nervous and neural, digestive and immune.
- Breathing exercises develop self-control and arbitrariness.
- Breathing is the foundation for persuasive public speaking, success in acting skills and singing. These bring along self-confidence and charisma.
- Children who work on their control of breathing are more relaxed, have better concentration skills and can more effectively regulate their moods.
- Children are much less susceptible to seasonal colds, bronchitis and bronchial asthma due to purification mechanisms occurring during breathing activities
- Breathing exercises in toddlerhood help to launch speech.
- For children with adenoids, asthma, cystic fibrosis or disorders of the cervical spine – blowing exercises are an essential part of physiotherapy. But exercises with such children require special care. Hence, it is better to entrust them to specialists.
- For children with autism and AD/HD – together with specialised guidance, regulated respiration games are effective correction tools to cope with frustration, emotional outbursts, self-regulation and speech development.
3. How are oral motor skills, breathing and language development related?
Oral motor skills relate to all movements in the mouth area, e.g. speaking, swallowing, laughing, sucking and chewing. Like any other motor skill, it must be developed, strengthened and actively promoted already since infancy. Oral motor skills are an important part of early language development.
A good interplay of tongue and lip movements is essentially responsible for the correct formation of sounds. The ability to coordinate the tongue and lips is particularly important for difficult sound combinations. These difficult sound combinations are called sibilants, and can be trained through playful exercises. For example, by learning to blow an object strongly or gently, thereby stretching the lips forward and preparing them for articulation.
4. Safety precautions during speech breathing play
❗️❗️ Do not openly display breathing toys and games due to small details and their potentially chocking hazards.
When starting an exercise, please ensure the following:
- Breathing activities should be done under adult supervision.
- Sterilise whistles and bamboo straws; or use disposable whistles and straws.
- Exercise in a dust-free, ventilated room with normal humidity.
- Play in optimal temperature between 17-21 degrees.
- Exercise before a meal or wait out for at least 1.5-2 hours after a meal.
- Wear comfortable clothes, no tight constraints.
- Do not over do it. If unwell, sleepy or with temperature, rather postpone the exercise.
- Make a plan and offer to do breathing exercises in such a way that the child feels systematicness and interactivity in terms of games’ variety.
- Carefully monitor the child’s well-being during exercises. If the child coughs heavily, complains of dizziness or general malaise, you should immediately stop and consult a doctor.
- A moderate blush is a healthy, natural effect and should not be frightening. If you notice some increase in breathing frequency – it’s also normal. Yet, monitor that it is not excessive, take breaks, alternate with calmer games. Moderate dizziness that soon stops is also a reaction within the normal range.
4.1. Real-case scenarios: what if the child is struggling to breathe during games?
VERY IMPORTANT! Breathing exercises are performed only in absolute comfort. Do not force breathing exercises. If introduced and re-introduced regularly, children tend to gradually discover more and more fun with breathing activities. Sometimes shorter sessions, sometimes longer ones.
4.1.2. Scenario 1
Observe the flow of air through the child’s nose. If the child does not have cold and seems to be healthy, yet the nose is still not allowing good airflow, then the child’s refusal may be due to some physical problem, discomfort, which he or she can not express or even realise. In this case, consult with your Paediatrician, who should ideally refer you to Otorhinolaryngologist. As early as possible.
Case in point C34. The child is 4 years old. The boy participates in short breathing games; longer activities lead to frustration. He has often a running nose, takes time to recover after colds, experiences difficulties to blow his nose. When healthy and asked spontaneously to breathe through his nose, does it with difficulty, gets frustrated. At night, the child is snoring. Mouth breathing is noticed during sleep and throughout the day. The boy swallows sounds in words, speaks too fast and is difficult to understand. After consultation with both the Paediatrician and Otorhinolaryngologist, he is diagnosed with adenoids in the nasal area and fluid buildup in his ears. An operation is recommended to remove adenoids and temporarily insert titanium tubes into the ears for airflow.
Successful post-operational results: the child uses his nose without problems and is always eager to participate in breathing activities. The child is also referred to have at least 24 sessions (45 mins each) with a speech therapist.
Thanks to the proactive steps of the parents to initiate and play breathing games – they were able to identify that something was wrong. They voiced their concerns to the specialists and corrected the problem in a timely manner.
4.1.3. Scenario 2
Another opposite scenario. When the child is overdoing it without noticing discomfort. For example, the child’s face turns pale, which may lead to fainting, or getting too red in the face. In this case, we recommend to monitor, stop and consult with the Paediatrician.
5. How to plan breathing exercises correctly?
- Plan as you like. Go through the list of the breathing games below and create your own routine.
- Increase the load gradually: start with simple tasks, then make them more difficult and longer.
- Always use a playful format.
TODDLERS
- Child neuro psychologists and psychologists recommend to start breathing exercises as of one year of age. In the form of play, in very short sessions, start with 30 seconds and increase to 2-3 minutes until the age of 3 years. As of 3-4 years, children grasp rules of breathing games more effectively and are ready to engage in more structured and longer breathing activities.
PRESCHOOLERS
- Filling up lungs with oxygen can quickly tire a child and may even lead to dizziness. Even though, it is not dangerous for a healthy child, we would recommend limiting the exercise to: 5-10 minutes on a daily basis.
Example 1. Regime’s duration for respiratory games: 2-15 minutes twice a day, for 2 weeks. Make a 1-month break. Then introduce another set of exercises for 2 weeks. And so on and so forth.
Example 2. Usually it depends on age and severity of the case. If it is a standard preventive practice, just integrate it into a daily life. Without schedules… Or why not make them a part of your morning exercises? This will be a great start to the day! There are so many scenarios for spontaneous play!
6. Foundational toys and games to train speech breathing
Educational breathing toys add a distinctive structure and interactivity to the breathing activity. We, at NeuroToys, offer you a refined selection of tested toys that deliver results. Have a look at the following:
- Show your magic with the Levitating Ball Game
- Launch the Wooden Boat with Balloon
- Get musical with Nose Flutes
- Be a star on the Football Table
- Be a train operator with the Wooden Whistle
7. Boost lung capacity with wind instruments (with caution)
It is definitely a big “YES” to have a set of toy wind instruments in your music corner at home.
However, when it comes to real wind instruments, then it takes effort to extract a sound. Some of them are so heavy, that only healthy children could learn to play them. When extracting the musical sound, the abdominal press is strongly strained and the intra-abdominal pressure increases.
Side note. It is usually not allowed to play a wind instrument if children have hernias and chronic diseases of the respiratory, cardiovascular system, digestive tract. Thus, consult a doctor before learning to play wind instruments.
7.1. At what age can children learn to play wind instruments?
The lungs experience the greatest stress when playing wind instruments. After all, a deep breath before blowing air into the instrument causes a strong stretching of lung tissue. After suffering from repeated inflammatory lung diseases, the elasticity of lung tissue usually decreases. In such cases, playing wind instruments can cause irreversible changes in lung tissue, leading to rupture of alveolar walls, emphysema of the lungs, etc.
Hence, it largely depends on the choice of instrument and requires individual approach to each child, taking into account his or her physical development and stamina. For instance, a child can be taught the flute from the age of 9, the oboe from the age of 10 or the clarinet from the age of 10-11. Moreover, for the initial training period one should buy a clarinet in E flat – the smallest in size. From 11-12 years old the child begins to learn to play the trumpet, from 12-13 years – the French horn, from 14 – bassoon, trombone and tuba.
7.2. Pros and cons of the saxophone
The saxophone is one of the most romantic instruments. To master the technique of playing, you need to have decent lungs and a good ear. The most common version of the saxophone is the viola. Usually it is the one that is taught to children, and after finishing a music school, entering a college or participating in a jazz band, they choose another timbre – baritone, soprano or tenor.
It is believed that playing the wind instruments helps a child to cope with ailments such as asthma or tonsillitis at an early stage of development. In addition, playing the saxophone develops the so-called “abdominal breathing”, which trains the abdominal muscles. Such breathing comes in handy in yoga and singing lessons. Best to start learning to play the saxophone is at the age of 10-12 years old when the body is mature and the lungs are stronger.
7.3. Pros and cons of the flute
The Flute – what a beautiful instrument with a “fluttering” sound. The most difficult moment at the beginning is to extract the first sound. If a future flutist is under 10 years old, consider buying a special J-shaped mouthpiece (head joint) for the instrument, because the straight mouthpiece can cause problems with your child’s shoulders and back. Once the basics are mastered, it won’t be a problem to switch to a flute with a straight mouthpiece.
The flute is recommended for children, particularly for those who have problems with the respiratory system. The point is that the flute requires deep inhale and exhale, which is the most intense aeration of the lungs and can benefit those prone to lingering bronchitis and colds, allergic respiratory conditions, as well as apathy and bad moods.
8. Basic blowing exercises to strengthen mouth, tongue and breathing muscles
We have put together a wide range of really cool exercises for you. They are easy to implement and they truly engage children on a systematic basis.
Please keep in mind. Some games require a quick frame of reference before the game starts and after it is finished. For example, playing with fire is not safe. Yet, we ask the child to blow out candles… Thus, a frame of reference is needed: “This is a special short game that we only play together…”. Or, another example, playfully licking a spoon during a meal, is not a good table manner. Hence, before you give a big spoon with a chocolate mouse on it, frame the situation, as in: “Do you want to play a short cool game with me?..”.
8.1. Breathing exercises that require minimum preparation
8.1.1. Part 1
- Blow out candles (as of 18 months).
- Use soap bubbles (start between 12-18 months).
Soap Bubbles are therapeutic and meditative. They have proved to be effective in coping with stress. For example, as of 12 months after a stressful visit to a doctor, encourage blowing the bubbles to calm down. Of course, chances that the child will be able to do it at this young age are very low, but it is a great early practice for emotional and breathing regulation.
- Puff out cheeks and press the cheeks simultaneously with hands or fingers to release the air. Adults usually press both cheeks for a small child. Do not repeat more than 3 times.
- Lick a spoon with something yummy on it.
- Eat long noodles by pulling them with the lips and the tongue.
- Next time when the mouth is dirty from a piece of cake, lick the upper and lower lips.
- Throw air kisses.
- Blow on paper or plastic windmill.
- Steam up glass of a window or a mirror with the warm airflow from the mouth (it better works in cold surroundings).
- Drink from the straw (occasionally – not often).
- Bubble blowing painting with straws.
- Sing songs.
- Learn poems.
- Inflate balloons (closer to 4 years). Did you know that it is highly recommended to inflate balloons for children with some respiratory issues and in post-recovery therapies?
Yet with CAUTION ❗️ especially until the age of 10 years!!! Balloons are the leading cause of suffocation death. Never leave children with uninflated balloons or even broken pieces of balloons. They are easily sucked into the throat and lungs and will make it impossible to breath.
8.1.2. Part 2
- Blow a feather, a leaf, mini DIY paper snowflakes
- Next time the tea is a bit hotter than usual, encourage to blow on the surface
- Explore scent – smell dandelions!
Example 1. Show your child a flower. Emphasise how good it smells! Invite your child to smell the flower, making sure the mouth is closed and that he or she breathes in through the nose.
Example 2. Show your child how to smell the flower and then make a “Mmmmmm” sound, as if you are enjoying the aroma. (Note: here you already introduce early sound activation necessary for speech breathing.)
Example 3. Offer other fragrant objects to smell. For example, perfume, soap, freshly baked goods. Wrinkle your nose as you exhale, if the object smells bad, harsh, unpleasant. For example, in case of garlic or onions.
- Blow onto a soft tissue and on a sheet of A4 paper. Hold a tissue out in front of the child. Ask to take a big breath in and blow onto the tissue/paper. If struggling, shorten the distance. Repeat three to four times.
- Use harmonicas and all types of whistles. Practice a strong force of exhalation! Then blow slowly into the whistle! Now alternate strong-weak-strong-weak exhalations, loud-quiet-loud-quiet exhalations.
Game suggestion. Offer to play hide-and-seek. The child hides and quietly whistles, whereas the adult is trying to guess the hiding spot.
- Fold lips into a tube and blow through the lips. To increase difficulty, fold lips into a tube, place a pencil between the nose and upper lip. Now breath through the nose only, ensuring the pencil is not falling down.
8.2. Gentle introduction to meditation – start early
Children need to learn how to cope with stress. These very simply exercises will teach children how to practice full inhalation and exhalation in a slow mindful way.
Mediation 1.
Stand with straight arms down and feet slightly apart. Slowly inhale, while raising the arms like wings above the head. Then slowly exhale, while bringing the arms back into the initial position. Repeat 10 times. Make combos: 1) breathe in and out ONLY through the nose; 2) breathe in through the nose, breathe out through the mouth.
Meditation 2.
In a sitting position, use only hands and fingers. On inhale spread the fingers wide open, on exhale, make fists. Repeat 10 times. Make combos: 1) breathe in and out ONLY through the nose; 2) breathe in through the nose, breathe out through the mouth.
Meditation 3.
Play a diver. The diver game trains the ability to hold a breath. The child takes two quiet inhales and two quiet exhales through the nose. And with the third deep breath, he or she closes the mouth and the nose with fingers, trying to hold the breath to the maximum. Another simple game option is to inhale as much air as possible, and hold the breath to the maximum. Repeat 5-10 times.
Meditation 4.
One nostril breathing. Stand up straight, body relaxed. Close the left nostril with your finger and take a deep, long breath through the nose. Open the nostril and close the right one, slowly exhale. Repeat 5-6 times. It is also important, that you also do it in reverse.
Meditation 5.
Teddy bear on the sea. In a lying position, place a soft toy on the chest. Inhalation and exhalation are done through the nose. The goal of the child is to raise and lower the toy via the mid-section breathing. Slowly up and down. Then place the toy on the tummy and ask the child to use abdominal breathing, so the toy goes up and down.
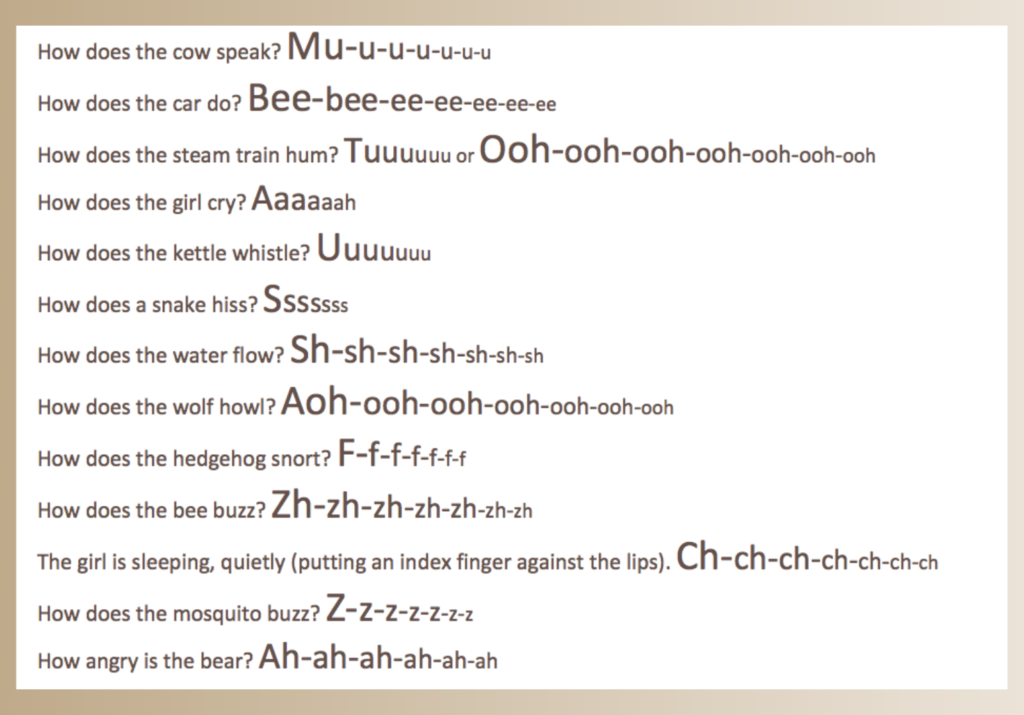
8.3. Exercises to activate speech breathing with sounds even before 12 months
Work on extended sounds
What will really help is a set of flash cards with objects and situations that imitate a unique sound. By linking objects and situations to sounds, you already help children to build associations and contexts early.
A rule of thumb – select sound imitations that are primarily aimed at “pulling out” vowels or long exhalations. Practice from greater to lesser intensity and from lesser to greater.
Here is a list of simple ideas to navigate you:
8.4. Embrace tongue-twisters
Pronounce on one full exhale – until you cannot say it anymore. Try to increase speed. Here are some cool examples in English:
Busy buzzing bumblebees.
Big nose, big blows.
Sing, ping, sling, pling.
A happy hippo hopped and hiccupped.
Selfish shellfish.
I am going to the gate; I will see you at eight. Don’t be late.
A big black bug bit a big black dog.
I saw a kitten eating chicken in the kitchen.
Birdie birdie in the sky laid a turdie in my eye.
A snake sneaks to seek a snack.
Fuzzy Wuzzy was a bear, Fuzzy Wuzzy had no hair. Then Fuzzy Wuzzy wasn’t fuzzy, was he?
8.5. Do-It-Yourself breathing activities that require longer preparation
Snowstorm in a bottle or in a cup
The game requires a straw, a clear transparent bottle or cup, a scotch tape and micro circles of paper from a hole puncher. If the bottle is used, make a hole in the cap and push the straw through. If without the cap, then use the scotch tape to moderately block the airflow. In case the plastic cup is used, a hole in the cover for the straw should be enough.
Goal in the box
The game requires cardboard, DIY pompoms, a chair, and a table. Take a small empty box. Prepare a mix of self-made paper balls, foil balls, cotton and wool balls. The weight of each type of balls will differ, and so will the strength of breathing. Use the carton box as a gate. To increase difficulty, close the box with a lid and cut out a medium-size gate for the balls to go through. Additionally, increase distance from the straw to the box. The goal is to move the balls across the table into the box by blowing through the straw.
Water bubbles in a glass
Next time the child is drinking juice or water, hand over a straw and suggest playing a short game to blow through the straw. Just make sure to set a frame of reference at the beginning “… this is only a game”. In case the child already discovered the concept, just let him or her enjoy it!
Scented jars
Prepare 5-6 safe-to-use jars. Fill them with different herbs. Smell. To heighten senses, use non-transparent jars. At first the child smells (without seeing substances), mentally evaluates and then visually associates the smell with the herbs form the jars. As an idea, consider using absorbent cotton balls for jars – which you can spray with child-friendly aroma oils. Why not try crushed substances, such as: coffee beans, mint, orange peels, pine, rose, etc.?
8.6. Auxiliary tools for children with health deviations
We highly encourage parents and child caregivers to gently introduce and regularly use breathing techniques through toys and DIY games from our comprehensive list. UNDER SUPERVISION.
However, it is important to keep in mind that a personalised approach to every child is detrimental. Embrace a trial and error approach, planning, observation and patience. Favouritism towards and rejection of some breathing exercises is individual. There is no extreme here. It is all a matter of time, place, cognitive readiness, weak oral motor skills, mood… age…
In other words, if today a parent asks a 3-year-old child with AD/HD to blow Ping-Pong balls on the table from position A to position B, it may not necessarily work. In this case, we encourage you for a re-trial in a few days, in 3 weeks, in 3 months, in 1 year, etc. Eventually, it will work. Consistency, playfulness and adherence to the rules are keys to successful results.
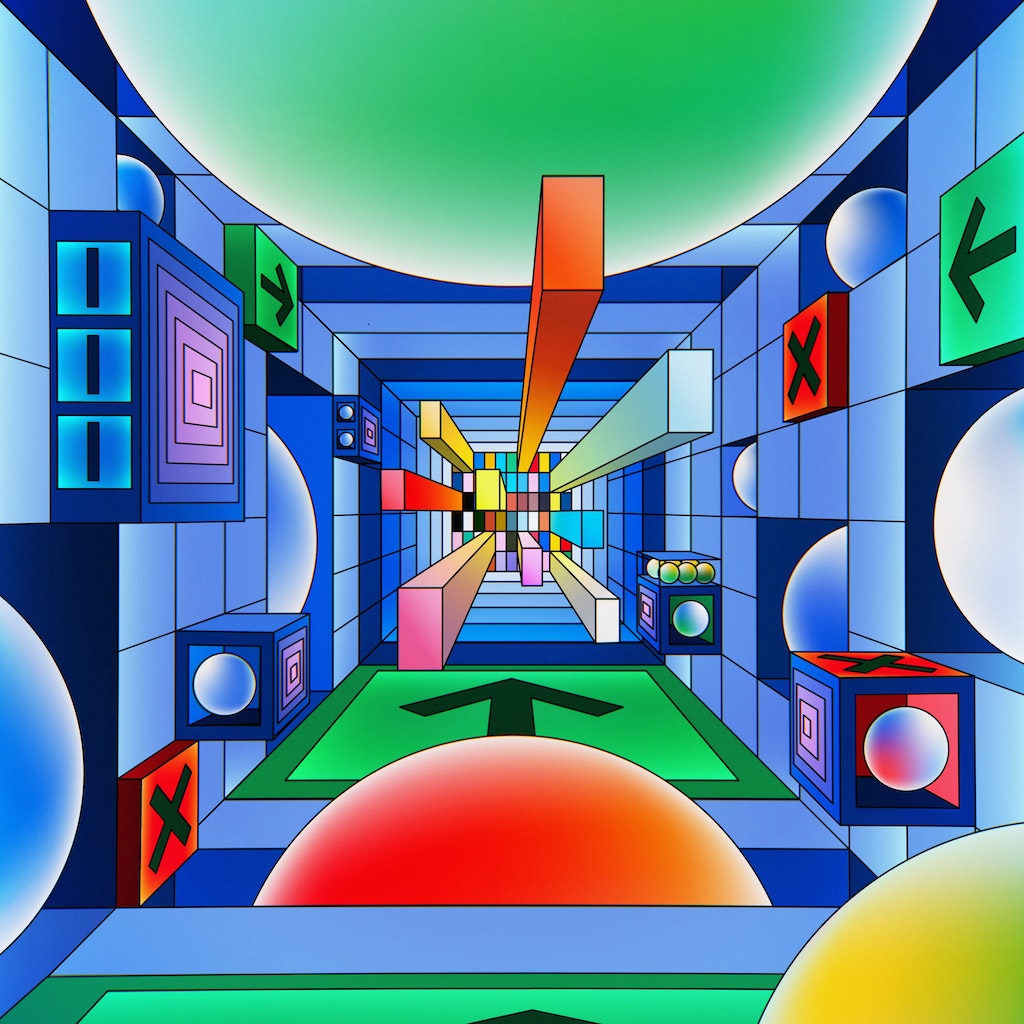
8.6.1. Video games for ADHD and asthma?
There are also specially designed screen biofeedback games. They support visual interactivity for children with AD/HD (Amon, K.L. & Cambell, A., 2008; Sonne, T. & Jensen, M.M., 2016) and even calm children down during blood drawing procedures (Sonne, T. et al, 2017). There are spirometry games to monitor asthma and facilitate prevention of asthma (van Delden, R. et al., 2020). It is easier for children to visualise, predict results and gain more self-awareness of own breathing. Spirometry offers multi-target incentives with real-time feedback. Just to tease you with a few examples:
“… a 30s breathing exercise showing a caterpillar going through an apple,.. a bee that flies over a fence via flowers,.. a sailboat that moves across a pond…“ (van Delden, R. et al., 2020)
These targets have different types of inhalation and exhalation tasks (shorter, longer, total, more forceful, quiet, etc.). Children interact, accomplish tasks, increase their lung capacity and train their control of breath.
9. 10 signs that a child may need a speech therapist
9.1. Standard amount of words on exhalation by age
The number of words on the exhalation is a characteristic of a child’s age. For example, at 2-3 years the norm is 2-3 words, and between 6 and 7 years – 5-7 words. Ideally, child experts recommend parents to observe speech development and seek therapy before the school starts, before the age of 7. Below you will find typical signs, if the child may require speech correction in the future.
One divides causes of speech defects and speech delays in children into two groups: biological and social. The first group clearly requires intervention by specialists at the beginning. The latter group is conditional and often correctional by therapy or disappears with age. This would depend on the individual characteristics of the child.
9.2. 10 signs to help recognise poor speech breathing and weak oral motor skills
9.2.1. Signs 1-5
Sign 1. An infant under one year of age has no humming or babbling at all, is silent or mooing inaudibly, and does not make the sounds typical of the early years such as “coos”, “oohs”, “ahhhs”, “bubu”, “tutu”, “yaya” etc. If this is your situation, then at one year of age the child needs a consultation not only from a speech therapist, but also from a neurologist.
Sign 2. In general, the optimal period for speech development is from 2 to 3 years. Yet, the child is already 2 years old, seems to understand everything, but is silent, or the vocabulary limits to about 10-12 words. A speech therapist knows how to stimulate speech in such kids offering a set of lessons. It does not hurt to take the child to the first consultation with a speech therapist.
Sign 3. The child seems to use mouth breathing throughout the day and while asleep (Hitos, S.F. et al., 2013). Early detection is critical!
Sign 4. A child who is over 3, active and quite motivated to speak. However, the child still speaks in his or her “bird’s” language: very few understandable words, mumblings, swallowing a lot of sounds. Then it’s time to see a speech therapist!
Sign 5. The child replaces words with other words completely dissimilar in sound: “baba” instead of “bunny”, “kika” instead of “car”, etc.
9.2.2. Signs 6-10
Sign 6. By this age, the phonetic system should be almost completely formed. The child speaks with firm articulation. Only a small percentage of problematic sounds might be present. Yet, the child turns 4-4,5, but instead of “cloud” he still says “kaud”, instead of “spoon” he says “fpoon”, instead of “like” he says “aik”… The child is soft with words… For example, this could be due to a psychological factor, where the child tries to draw attention to himself or herself from adults or caused by dysarthria.
Sign 7. The child talks too fast or, on the contrary, with hesitations, pauses, repeating the first sounds, syllables and words, i.e. stuttering.
Sign 8. A 6-year-old child does not memorise poems, cannot retell a short text, breaks the structure of words, skips syllables in long words, and swallows endings.
Sign 9. The child struggles to burr – make a strong pronunciation of the ‘r’ trembling sound.
Sign 10. The young school child has small vocabulary and has trouble writing, too much jumbling, poverty of speech.
10. Concluding takeaways on speech breathing
Training of breathing goes hand in hand with the development of speech. The quality of our speech depends on how well we breathe in and out. With untrained speech breathing in early childhood, children will face problems: inability to speak long sentences, incorrect intonation, incomprehensible speech, difficulties to learn a poem, poor vocabulary, outcast from social circles, difficulty to make friends, etc.
Yet, to date, there is a plethora of respiratory toys and games that effectively help to train breathing speech before even a child turns 1 year.
If parents pay attention to training speech breathing in the toddlerhood and preschool period, there is a very high chance to prevent speech disorders and increase chances of successful performance in a kindergarten and at school.
The good news is that refinement of the speech breathing mechanism is in many cases possible. It requires gradual correction work and it is most effective in healthy 3- to 10-year-old children (Boliek C.A. et al, 2009). What matters is that parents choose sets of exercises through each year, plan them ahead and practice regularly. By doing this groundwork with children, they mindfully and playfully strengthen their respiratory system and help them build articulate speech.
Chew more healthy snacks with different textures! Participate in a variety of breathing exercises! And next time, a ladybug ends up on your hand, make a wish and blow on it together with your child!
Let’s lay down foundation for speech breathing in a timely and mindful manner, and develop a joy in speaking early!
P.S.: all the afore-mentioned toys and games are highly recommended for improving cognitive and respiratory functions of older people and in individuals in rehabilitation after stroke, concussion and surgery.
REFERENCES
Amon, K.L. & Cambell, A. (2008) “Can Children with AD/HD Learn Relaxation and Breathing Techniques Through Biofeedback Video Games?”. Australian Journal of Educational & Developmental Psychology, Volume 8, pp. 72-84.
Boliek C.A., Hixon, T.J., Watson, P.J., & Jones, P.B. (2009) “Refinement of Speech Breathing in Healthy 4- to 6-year-old Children”. Journal of Speech, Language, and Hearing Research, Aug, 52 (4), pp. 990-1007.
Fuchs, S. & Rochet-Capellan, A. (2021) “The Respiratory Foundations of Spoken Language”. Annual Review in Linguistics, 2021 7 (1), pp. 13-30.
Hitos, S.F., Arakaki, R., Soléc, D. & Weckx Luc L.M. (2013) “Oral Breathing and Speech Disorders in Children”. Jornal de Pediatria (Rio J), 89 (4), pp. 361-365.
Hoit, J.D., Hixon, T.J., Watson, P.J. & Morgan, W.J. (1990) “Speech Breathing in Children and Adolescents.” Journal of Speech and Hearing Research, 33 (1), pp. 51-69.
Muacevic, A. & Adler, J. (2018) “The Influence of Breathing on the Central Nervous System”. Cureus, June, 10 (6), e2724.
Sonne, T. & Jensen, M.M. (2016) “ChillFish: A Respiration Game for Children with AD/HD”. TEI 2016, February 14-17.
Sonne, T., Merritt, T., Marshall, P., Lomholt, J.J., Müller, J. & Grønbæk, K. (2017) “Calming Children When Drawing Blood Using Breath-Based Biofeedback”. In Proceedings of the 2017 Conference on Designing Interactive Systems (Edinburgh, United Kingdom) (DIS ’17). Association for Computing Machinery, New York, NY, USA, pp. 725-737.
van Delden, R., Bos D. P-O., Vivian (Vivianne) de With, A.J., Vogel, K., Klaassen, R., Zwart, N., Faber, J., Thio, B. & van der Kamp, M. (2020) “SpiroPlay, a Suite of Breathing Games for Spirometry by Kids & Experts”. CHI PLAY ’20, November 2–4, 2020, Virtual Event, Canada.